Utilization Review
What is Utilization Review?
Utilization Review in Michigan is a new process (as of December 2020) through which insurers can challenge the reasonableness and necessity of medical services provided under the Michigan No-Fault Act.
Utilization Review is established by MCL 500.3157a. The rules and regulations for Utilization Review have been promulgated by the Michigan Department of Insurance and Financial Services. The rules can be found at this link.
How does Utilization Review work?
If an insurer believes that a medical provider has overtreated or treated over-aggressively, it can deny the provider’s bills and then ask the Michigan Department of Insurance and Financial Services “DIFS” for a ruling on the same.
What is the process for Utilization Review?
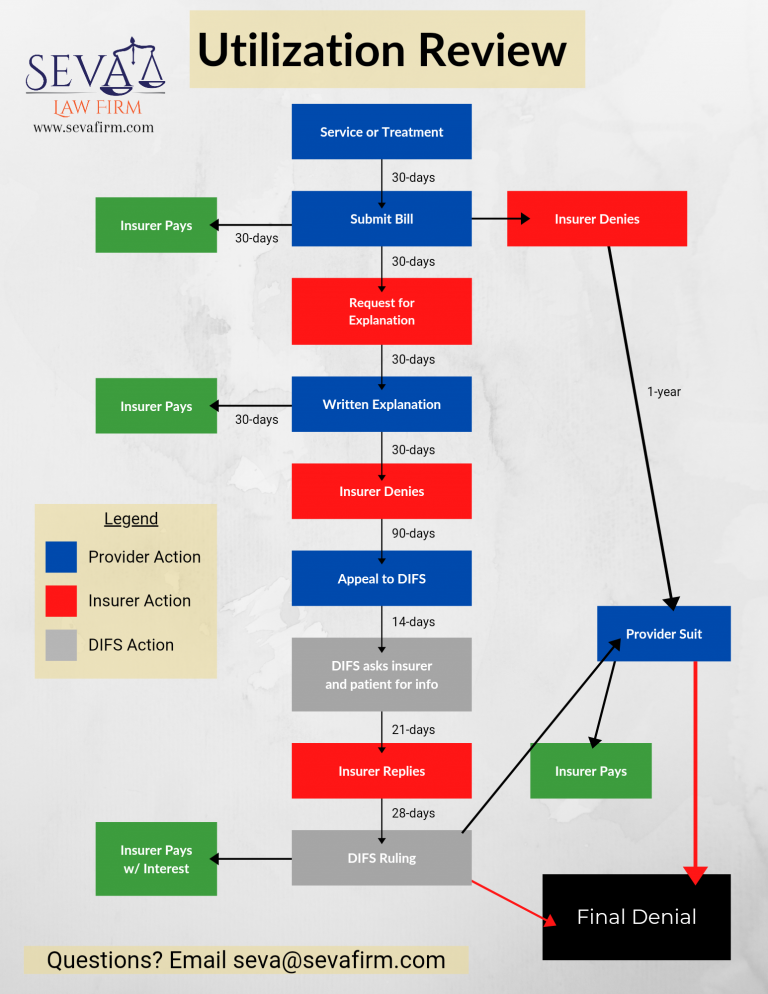
The below flowchart provides the steps and time frames for the Utilization Review process.
Does a provider have to go through Utilization Review if its bill is denied for overtreatment or unreasonable treatment?
No. Utilization Review is not an exclusive remedy. A provider may file a provider suit pursuant to MCL 500.3112 at almost any time during the process.
Is there a benefit for going through the Utilization Review?
As a medical provider, there are two benefits to going through Utilization review: (1) It is faster than going through a medical provider lawsuit and (2) if you win, you are guaranteed 12% interest.
More questions about Utilization Review?
Call 248-385-5704 or email [email protected]